A New Chapter in Spine Care
When I started my career as a neurosurgeon, the standard approach for treating severe degenerative disc disease was spinal fusion. At the time, it was our best option. By permanently joining two vertebrae together, we could stabilize the spine, relieve pain, and prevent further damage.
The problem? Fusions limit mobility. Patients often felt better after surgery, but they also noticed stiffness and reduced flexibility. Over time, some even developed new issues in the discs above and below the fusion site — a complication we call adjacent segment disease.
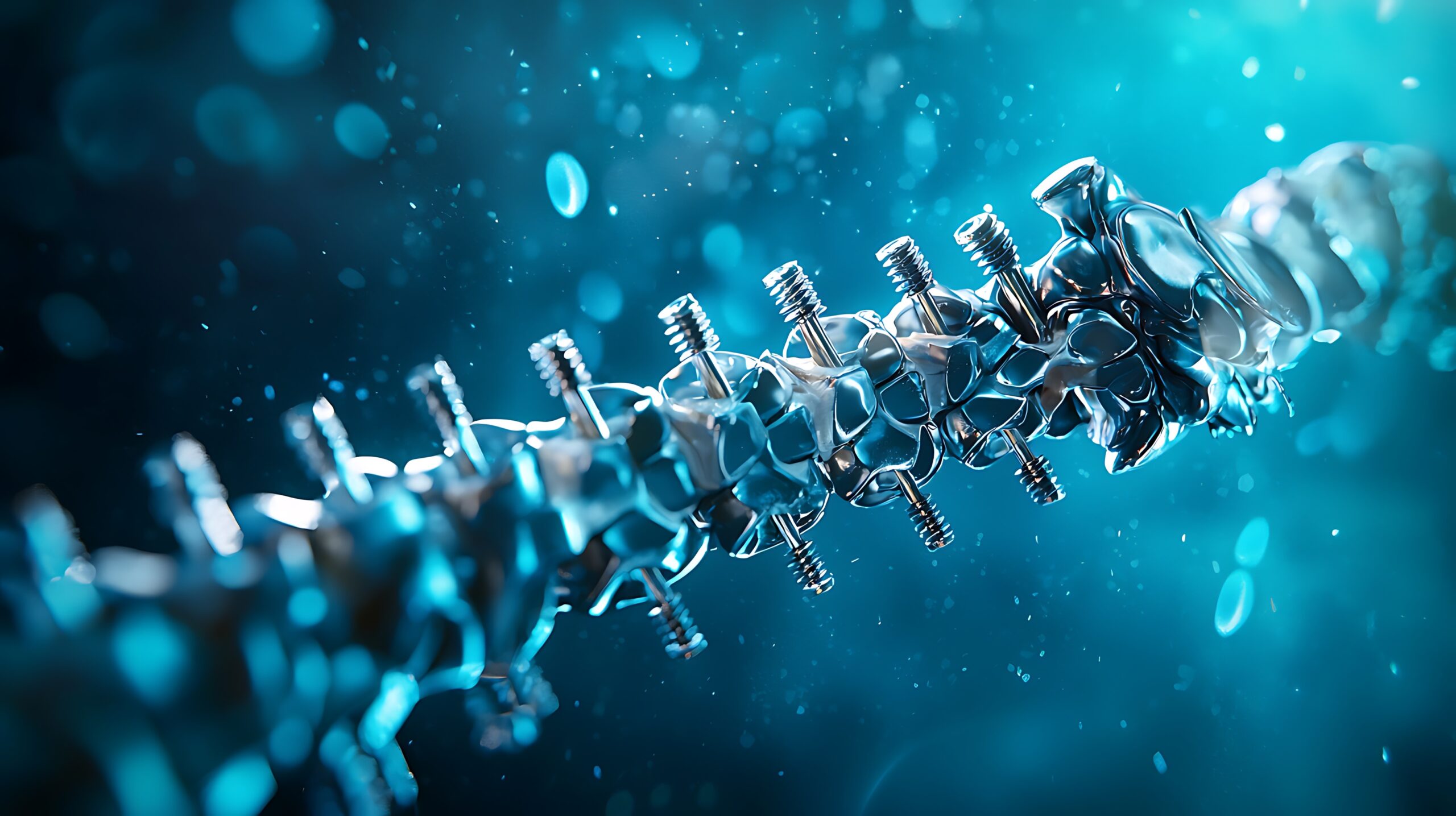
That challenge led to the development of artificial disk replacement (ADR) — a technology that has evolved dramatically over the past two decades. Today, thanks to advanced materials, better biomechanical designs, and long-term data, artificial disks are helping patients get back to living pain-free and fully mobile lives.
Why Artificial Disks Are a Game-Changer
Artificial disk replacement is designed to preserve natural motion in the spine — something fusions simply can’t do. Instead of removing the damaged disk and locking the bones together, we replace it with a biomechanical implant that mimics the natural structure and movement of a healthy disk.
For patients, this means:
- Better flexibility compared to fusion
- Reduced stress on nearby spinal levels
- Faster recovery and quicker return to daily activities
- Improved long-term outcomes
I’ve performed many ADR procedures, and time and again, I’ve seen patients regain not just their movement but also their confidence — the freedom to bend, twist, and live without constant pain.
The Evolution of Disk Design
When artificial disks were first introduced, the designs were fairly basic — often rigid, metal-based implants. While they helped some patients, early models had limitations. They didn’t perfectly replicate the spine’s natural biomechanics, and wear-and-tear over time was a concern.
Today, things look very different. The latest generation of artificial disks focuses on flexibility, durability, and adaptability:
- Advanced Materials: Modern disks combine titanium endplates for strength with polyethylene cores that allow smooth, controlled motion. These materials are lightweight, durable, and biocompatible, meaning the body tolerates them well.
- Motion Preservation Technology: Newer implants are designed to mimic the exact range of motion of a natural disk — flexion, extension, lateral bending, and rotation — helping the spine move as close to normal as possible.
- Wear-Resistant Coatings: Engineers have introduced surface coatings that reduce friction and prevent debris from forming over years of use, which extends the life of the implant.
These design improvements mean patients can expect better function, fewer complications, and longer-lasting results than ever before.
Biomechanics at the Core
One of the most exciting parts of this field is how closely we’re now matching the natural mechanics of the spine.
The spine is a remarkable structure — strong enough to support our entire body weight yet flexible enough to allow motion in multiple directions. An effective artificial disk needs to recreate this delicate balance.
Through 3D modeling, robotic-assisted surgery, and finite element analysis (a form of computerized stress testing), we’re now able to design implants that distribute forces evenly across the spine, just like a healthy disk would.
The result? Less strain on surrounding vertebrae and reduced risk of complications years down the line.
Long-Term Success Rates
Whenever I talk to patients about artificial disk replacement, one of the first questions they ask is:
“Will this last?”
It’s a fair concern — especially since spinal implants are meant to support decades of use. Fortunately, long-term data on modern ADR devices is extremely encouraging.
Studies are showing success rates above 90% for pain relief, mobility restoration, and patient satisfaction — even 10 to 15 years after surgery. Better yet, these patients often avoid some of the complications associated with fusion, such as adjacent segment disease.
In my own practice, I’ve seen patients return to sports, active work, and hobbies within months of recovery. For many, the surgery doesn’t just fix their spine — it gives them their life back.
Robotics and AI: The Next Leap Forward
Another advancement revolutionizing ADR is the integration of robotic-assisted surgery and artificial intelligence.
With robotic systems, we can plan each procedure with millimeter-level precision, ensuring the implant is perfectly aligned with the patient’s unique anatomy. This level of accuracy improves outcomes, reduces recovery time, and lowers the risk of complications.
AI is also helping us analyze long-term patient data to predict which implants will work best for specific individuals based on factors like spinal alignment, bone density, and lifestyle. Personalized medicine is becoming a reality in spinal surgery, and artificial disks are at the forefront of that shift.
Who’s the Right Candidate?
Not every patient with back pain needs or qualifies for artificial disk replacement, and part of my role is helping people understand their options. Generally, the best candidates are those who:
- Have degenerative disk disease limited to one or two levels of the spine
- Have not responded to conservative treatments like therapy, medication, or injections
- Want to maintain mobility and avoid spinal fusion if possible
For others — particularly patients with extensive degeneration, instability, or significant nerve compression — fusion may still be the better option. The key is matching the right treatment to the right patient.
Redefining What’s Possible
Artificial disk replacement has evolved from an emerging technology into a proven, highly effective solution for many patients suffering from chronic neck or lower back pain.
We’re no longer simply focused on stabilizing the spine; we’re restoring its natural function. That shift — from limitation to mobility — is changing lives every day.
I believe we’re just scratching the surface of what’s possible. With smarter materials, improved biomechanics, robotics, and data-driven personalization, the next generation of artificial disks will only get better, safer, and longer-lasting.
For patients who’ve been told they’ll have to “learn to live with pain,” I can tell you: there’s real hope on the horizon.